Egg Freezing: Benefits, Procedures, and What to Expect
Introduction
Egg freezing, also known as oocyte cryopreservation, has revolutionized family planning for women across the globe. This innovative fertility preservation technique allows women to extend their reproductive timeline by freezing their eggs during their most fertile years for potential future use. As more women delay childbearing to pursue education, career goals, or await the right partner, egg freezing has emerged as a powerful option that provides greater reproductive autonomy and choice.
The decision to pursue egg freezing is deeply personal and often influenced by various factors including age, relationship status, career demands, and medical conditions. Whether you’re considering egg freezing for medical reasons or as a proactive approach to family planning, understanding the benefits, procedures, and expectations is crucial.
This comprehensive guide will walk you through everything you need to know about the egg freezing process, from initial consultation to post-procedure care, helping you make an informed decision about your reproductive future.
What is Egg Freezing?
Egg freezing is a medical procedure that involves harvesting eggs from a woman’s ovaries, freezing them in a laboratory, and storing them for potential future use. The scientific term for this process is oocyte cryopreservation, which literally means preserving eggs at extremely low temperatures.
During a woman’s reproductive years, particularly in her 20s and early 30s, her eggs are typically healthier and more viable. By freezing eggs during this optimal period, women can essentially “pause the biological clock” on their eggs, preserving them in their current state for future use. When a woman is ready to use her frozen eggs, they can be thawed, fertilized with sperm in a laboratory through a process called in vitro fertilization (IVF), and the resulting embryos can be transferred to her uterus.
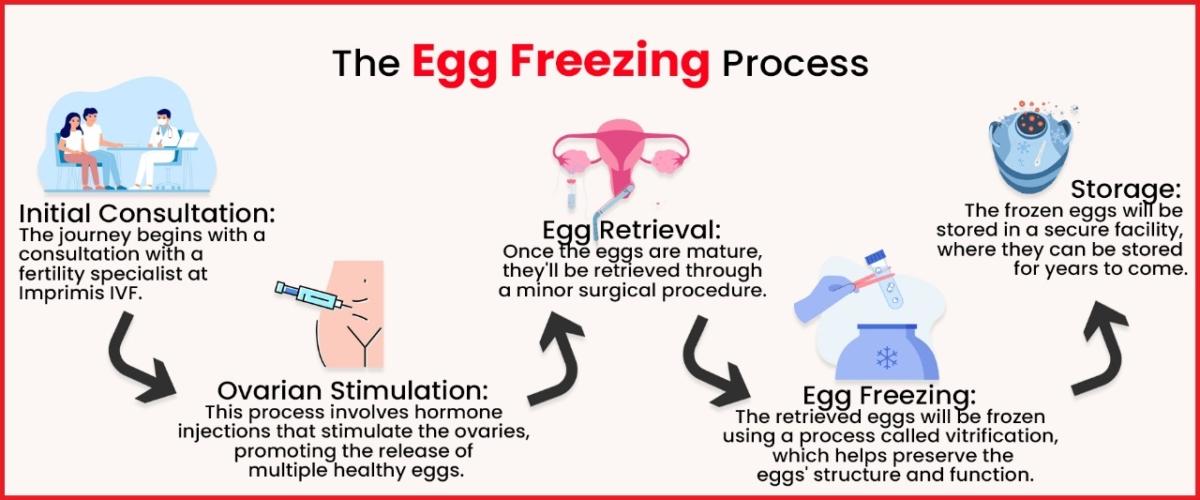
The egg freezing process involves several stages:
- Consultation and Testing: Initial assessment of ovarian reserve and overall health
- Ovarian Stimulation: Hormone injections to stimulate the ovaries to produce multiple eggs
- Egg Retrieval: A minor surgical procedure to collect the eggs
- Freezing: Vitrification (flash-freezing) of the collected eggs
- Storage: Long-term preservation of the eggs in specialized facilities
Benefits of Egg Freezing
Preserving Fertility for Medical Reasons
One of the primary benefits of egg freezing is for women facing medical treatments that may compromise their fertility. Treatments such as chemotherapy, radiation, or certain surgeries can potentially damage the ovaries and affect egg quality and quantity. For these women, egg preservation through freezing offers hope and the possibility of having biological children after recovery.
Cancer treatments, in particular, can be devastating to fertility. By freezing eggs before beginning cancer treatment, women can significantly increase their chances of having biological children later. This application of egg freezing technology has been transformative for many cancer survivors who might otherwise have lost the ability to have genetic offspring.
Extended Reproductive Timeline
For women not yet ready to start a family, the egg freezing process provides the opportunity to extend their fertile years. While natural fertility begins to decline in a woman’s early 30s and drops more significantly after 35, frozen eggs remain at the quality they were when harvested. This means a woman who freezes her eggs at 32 can potentially have the same chance of pregnancy with those eggs when she’s 42 as she would have had at 32 using fresh eggs.
The ability to preserve fertility while pursuing educational or career goals has been particularly valuable for many professional women. It reduces the pressure to choose between career advancement and family planning within a limited timeframe.
Greater Control and Reduced Pressure
Egg freezing offers women more control over their reproductive timeline, reducing the pressure to find a partner or start a family before they’re ready. This freedom from the “biological clock” can allow for more authentic relationship development and life choices without the constant anxiety about diminishing fertility.
Many women report that after completing the egg freezing process, they feel a sense of relief and empowerment. Having a “backup plan” allows them to approach other life decisions with greater confidence and less reproductive pressure.
Increased Pregnancy Success in Later Years
Using eggs that were frozen during a woman’s more fertile years can significantly increase the chances of successful pregnancy in her late 30s or 40s compared to using eggs that have aged along with her. This is because egg quality naturally declines with age, increasing the risk of chromosomal abnormalities and decreasing implantation rates.
Statistics show that while the success rate of IVF with fresh eggs drops dramatically after age 35, the success rate using eggs frozen at a younger age remains relatively stable, reflecting the age at which the eggs were frozen rather than the woman’s current age.
Who Should Consider Egg Freezing?
Age Considerations and Egg Freezing Age Limit
While there’s technically no strict upper egg freezing age limit, most fertility specialists recommend freezing eggs before age 35 for optimal results. The quality and quantity of eggs begin to decline in a woman’s early 30s, with a more significant drop after 35. Women between 25-35 years old typically have the best outcomes in terms of egg quality and quantity retrieved.
That said, egg freezing can still be beneficial for women in their late 30s or early 40s, though they may need multiple cycles to retrieve an adequate number of eggs and should have realistic expectations about success rates. Most clinics have an upper age limit of around 40-45 years for egg freezing procedures, based on diminishing returns beyond this age.
Medical Indications
Women diagnosed with conditions that may affect fertility should consider egg freezing as early as possible. These conditions include:
- Cancer requiring chemotherapy or radiation
- Autoimmune disorders requiring treatments that could affect fertility
- Endometriosis
- Primary ovarian insufficiency
- Need for ovarian surgery
- Genetic conditions that may cause premature ovarian failure
For these women, egg preservation through freezing may be their best option for having biological children in the future.
Personal Circumstances
Beyond medical reasons, many women choose egg freezing for social or personal reasons:
- Pursuing educational or career goals
- Not yet having found a partner
- Not feeling ready for parenthood
- Partner not ready for children
- Same-sex female couples who both wish to have a genetic connection to their children
Whatever the reason, egg freezing provides options and time for women to make reproductive choices aligned with their life circumstances and personal values.
The Egg Freezing Process: Step by Step
Initial Consultation and Testing
The egg freezing journey begins with a comprehensive consultation with a reproductive endocrinologist. During this appointment, the doctor will:
- Review your medical history
- Perform a physical examination
- Order blood tests to check hormone levels related to fertility
- Conduct an ultrasound to assess your ovarian reserve (the quantity of eggs remaining in your ovaries)
- Discuss your goals, expectations, and the realistic outcomes of the procedure
This evaluation helps determine if you’re a good candidate for egg freezing and what protocol might work best for your specific situation. The doctor will also discuss the costs, risks, and expected timeline for the process.
Ovarian Stimulation
Once you decide to proceed with egg freezing, the next step is ovarian stimulation. Normally, a woman’s body releases one egg per month. For egg freezing to be efficient, multiple eggs need to be retrieved in a single cycle. To achieve this:
- You’ll begin taking hormone medications (gonadotropins) via self-administered injections for approximately 8-12 days
- These hormones stimulate your ovaries to develop multiple follicles containing eggs
- Regular monitoring through blood tests and ultrasounds will track the development of these follicles
- When the follicles reach optimal size, a “trigger shot” of hCG or GnRH agonist is administered to finalize egg maturation
During this phase, you may experience some side effects such as bloating, mood swings, breast tenderness, or discomfort at injection sites. Most women continue their normal daily activities during stimulation, though strenuous exercise is typically discouraged.
Egg Retrieval Procedure
Approximately 36 hours after the trigger shot, the egg retrieval procedure takes place. This is a minor surgical procedure performed under light sedation or anesthesia:
- The procedure typically takes 15-20 minutes
- Using ultrasound guidance, the doctor inserts a thin needle through the vaginal wall into each ovarian follicle
- The fluid containing the eggs is aspirated through the needle
- An embryologist immediately identifies and counts the eggs retrieved
- The procedure is done on an outpatient basis, meaning you can go home the same day
Most women experience some cramping, bloating, or spotting for a few days following retrieval. Serious complications are rare but can include bleeding, infection, or ovarian hyperstimulation syndrome (OHSS), a condition where the ovaries become swollen and painful.
Freezing and Storage
Once the eggs are retrieved, they’re immediately evaluated by the embryology team:
- Mature eggs are identified and prepared for freezing
- The eggs undergo vitrification, an ultra-rapid freezing process that prevents ice crystal formation
- Vitrified eggs are stored in liquid nitrogen at -196°C (-320°F)
The vitrification process has revolutionized egg preservation, dramatically improving survival rates of eggs after thawing compared to older slow-freezing methods. Properly vitrified and stored eggs can theoretically remain viable indefinitely, though most research confirms effectiveness for at least 10-15 years.
Storage fees typically range from $500-$1,000 per year, depending on the facility. Some women choose to store their eggs at the clinic where they were retrieved, while others opt to transfer them to long-term storage facilities that may offer lower annual fees.
Success Rates and Realistic Expectations
Understanding success rates is crucial when considering egg freezing. Several factors influence the likelihood of eventually achieving pregnancy with frozen eggs:
Age at Freezing
The woman’s age when her eggs are frozen is the single most important factor affecting future success rates. Eggs frozen before age 35 have significantly higher success rates than those frozen at later ages. According to recent studies:
- Women under 35: Approximately 50-60% chance of a live birth from one round of egg freezing (if 15-20 eggs are retrieved)
- Women 35-37: About 40-50% chance
- Women 38-40: About 30-40% chance
- Women over 40: Less than 30% chance
These statistics underscore why fertility specialists recommend egg freezing earlier rather than later for optimal outcomes.
Number of Eggs Retrieved and Frozen
The number of eggs retrieved in a cycle varies widely based on age, ovarian reserve, and response to stimulation medications. Generally:
- Women under 35 typically produce 15-20 eggs per retrieval cycle
- Women over 35 may produce fewer eggs, often requiring multiple cycles
Most specialists recommend having at least 15-20 mature eggs frozen to have a reasonable chance at one live birth. Women freezing eggs after 35 may need multiple cycles to reach this number.
Clinic Success Rates
Success rates vary between clinics based on their experience with egg freezing, laboratory techniques, and quality control measures. When selecting a clinic, it’s important to ask about:
- Their specific experience with egg freezing
- Egg survival rates after thawing
- Fertilization rates with thawed eggs
- Pregnancy and live birth rates from thawed eggs
Clinics with more experience and better laboratory protocols generally have higher success rates.
The Future Use of Frozen Eggs
When a woman decides to use her frozen eggs, the process involves:
- Thawing: The eggs are carefully thawed using specialized protocols to maximize survival rates
- Fertilization: Thawed eggs are fertilized through intracytoplasmic sperm injection (ICSI), where a single sperm is injected directly into each egg
- Culture: Successfully fertilized eggs develop into embryos in the laboratory for 3-5 days
- Testing (optional): Embryos can undergo preimplantation genetic testing (PGT) to screen for chromosomal abnormalities
- Transfer: One or two of the healthiest embryos are transferred to the woman’s uterus
- Pregnancy test: Conducted approximately two weeks after embryo transfer
Any additional healthy embryos can be frozen for potential future use.
The success of this process depends on many factors, including the quality of the eggs after thawing, successful fertilization, embryo development, and the woman’s uterine health at the time of transfer.
Emotional and Psychological Aspects
The egg freezing journey can be emotionally complex. Women pursuing egg freezing often experience:
- Relief and reduced anxiety about their reproductive timeline
- Empowerment from taking proactive steps regarding their fertility
- Stress related to the medical procedures and financial investment
- Emotional ups and downs from hormone medications
- Complex feelings about aging, relationships, and family planning
Many fertility clinics offer psychological support services or can refer patients to specialized counselors familiar with fertility issues. Support groups, both in-person and online, can also provide valuable emotional support from others going through similar experiences.
Conclusion
Egg freezing represents a significant advancement in reproductive technology, offering women more options and greater control over their fertility timeline. Whether pursued for medical preservation or personal choice, the egg freezing process provides a potential path to future parenthood that wasn’t available to previous generations.
As with any medical procedure, egg freezing comes with no guarantees. However, for many women, the possibility it offers—extending their fertile years and preserving the option of genetic motherhood—makes it a worthwhile consideration despite the costs and medical procedures involved.
If you’re considering egg freezing, consult with a reproductive endocrinologist who specializes in fertility preservation to discuss your specific situation, including your age, ovarian reserve, and personal goals. With the right information and expectations, you can make an informed decision about whether egg freezing is the right choice for your reproductive future.
FAQs About Egg Freezing
Q: What is the ideal age for egg freezing? A: While there’s no one perfect age, most specialists recommend egg freezing before age 35 for optimal egg quality and quantity. The earlier the eggs are frozen, generally the better the outcomes.
Q: How many eggs should I freeze? A: Most fertility specialists recommend freezing 15-20 mature eggs to have a reasonable chance at one live birth. Women over 35 may need to undergo multiple cycles to retrieve this number.
Q: How long can eggs remain frozen? A: Theoretically, eggs can remain frozen indefinitely. Studies have confirmed successful pregnancies from eggs frozen for 10-15 years, and there’s no known biological reason why properly stored eggs would not remain viable longer.
Q: Will the hormones used in egg freezing cause weight gain? A: Some women experience temporary weight gain (typically 2-5 pounds) due to water retention during the stimulation phase, but this generally resolves within a week or two after the procedure.
Q: Does egg freezing affect my natural fertility? A: No, egg freezing does not diminish your natural fertility. The procedure retrieves eggs that would have been lost during that month’s menstrual cycle anyway.
Q: What happens if I never use my frozen eggs? A: If you conceive naturally or decide not to use your frozen eggs, you typically have several options: you can continue storing them, discard them, donate them to research, or donate them to another woman struggling with infertility (though this requires additional screening).
Q: Can I use my frozen eggs with any partner? A: Yes, frozen eggs can be fertilized with sperm from any partner or donor of your choosing when you decide to use them.
Q: What risks are associated with egg freezing? A: The main risks include ovarian hyperstimulation syndrome (OHSS), infection, bleeding, or reaction to anesthesia during retrieval. Serious complications are rare, occurring in less than 1% of cases.